The British neuroscientist Adrian Owen has developed ways to connect with patients in a vegetative state. It’s amazing work — with complicated implications.
Adrian Owen has been studying the minds of vegetative patients for more than two decades, and to this day their flashes of awareness astound him. “They are often laying down memories just like you and I are,” he says. “They’re experiencing emotional pain, they have hopes for the future, they have memories of the past.” It turns out, the human mind doesn’t work like a light switch. Even a severely damaged brain can still sometimes blaze with thoughts; it’s just that these flickers might only occur with the right stimulus. That’s where Owen’s work comes in. As the head of the Owen Lab at Western University in Ontario, Canada, he has devised a brain-scanning technique that enables vegetative patients to answer questions simply by thinking (TEDxUWO Talk: The quest for consciousness). The science is still in its infancy, and Owen’s techniques are rarely practiced beyond the confines of his lab. We asked him to explain how his work might help some of the world’s vegetative patients break their silence.
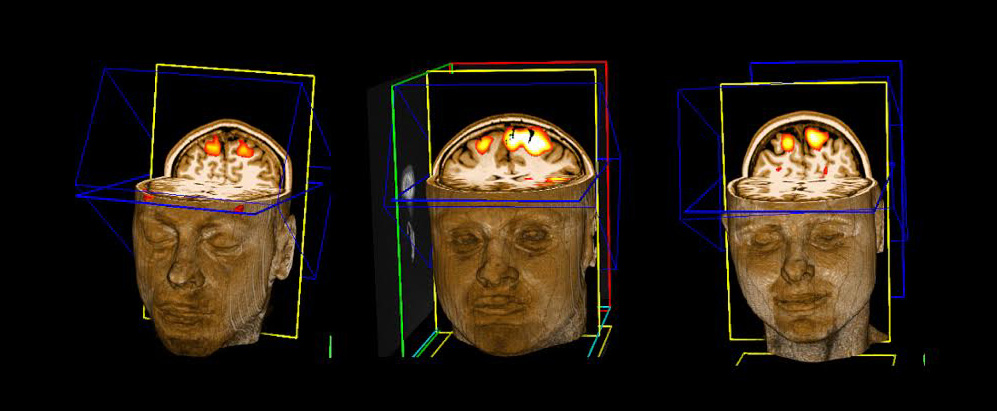
Communication begins with an imaginary game of tennis. If you picture yourself playing tennis, a dense network of synapses begins firing along the top of your brain; an MRI scan will show a distinct patchwork of glowing blobs. Owen used this pattern to reach through to patients who could not speak, move or blink on command. He instructed his first patient, a woman who had been unresponsive for five months, to imagine a game of tennis. Right on cue, the telltale blobs appeared on screen. “Bingo; she was conscious,” he says. And she was far from alone. Subsequent experiments showed that roughly one in five patients could respond to Owen’s prompts, and the healthiest among them could answer a series of “yes” or “no” questions. In lieu of saying “yes,” they imagined tennis instead.
Wait. One in five vegetative patients might, in fact, be conscious? Truthfully, it’s a tentative estimate. Owen’s brain scans are not standard practice, so he’s drawing conclusions from a frustratingly small pool of patients numbering in the several hundreds. The vast majority of vegetative patients are still diagnosed the old fashioned way — with a clap behind the ears or a finger running past the eyes. While Owen’s breakthroughs have grabbed headlines, he suspects it will take a number of years before they become standard clinical practice. “These things are not decided by scientists,” he says, “They’re decided by, you know, task forces and the Royal College of Physicians in the UK and boards of physicians who maybe meet every ten years to reevaluate the diagnostic criteria.”
Tennis wasn’t arbitrary. It was a surefire communication starter. It took Owen roughly ten years to alight on the tennis test for MRI scanners (he also experimented with asking patients to remember Christmas carols and pictures of faces). But tennis proved most effective because it worked up such an unmistakable pattern in the brain’s premotor cortex, which processes movement. The elaborate choreography of gripping the racket and racing toward the ball lit up the same region of the brain from one patient to the next. Nonetheless, it’s painstaking, strenuous work. Patients have to travel to London, Ontario for five days, where Owen challenges them to imagine tennis for 30 seconds at a time, ten times in a row. “I do it ten times just because by the end of the tenth 30-second period we are 100% sure the person is responding,” Owen says. That’s a burden even for a healthy brain.
One patient, a lifelong hockey fan, was spared from watching endless reels of hockey games when he revealed that he had had enough.
Not into tennis? Try Alfred Hitchcock. Owen has also gauged awareness by screening an 8-minute edit of Alfred Hitchcock’s television program, Bang! You’re Dead. In the episode, a young boy mistakes a revolver for a toy gun. If the patient shows a surge of mental activity during tense dialogue, that might mean speech perception is intact. A spike at the moment the boy points the gun at the camera suggests a lively visual cortex. “We can actually tell quite a lot about somebody’s brain function based simply on the patterns of changing brain activity over the course of a short Alfred Hitchcock movie,” Owen says.
A new technique: using a portable EEG machine. To reach more patients, Owen recently bought a jeep and a portable electroencephalogram machine, which includes a cap of electrodes that attach to a patient’s skull. A team of researchers regularly drive the “EEJeep” across Ontario to meet patients in their homes to use a similar technique to the MRI machine. Nonetheless, the new machine poses a thicket of challenges for the research, chiefly that it does not penetrate the deepest reaches of the brain. As a result, the team has to devise a new set of questions that activates neurons closer to the surface. Owen estimates it will take another five years to find an equally effective readout through EEG. But he is excited at the idea’s potential, not least because EEG machines are far cheaper to operate than MRI machines. If the technique proves successful, Owen and his team could have a cost-effective blueprint for hospitals and clinics around the world.
They won’t ask patients whether they want to live or die until legal experts and ethicists have hashed out the issues.
The types of questions that can be asked are strictly supervised … On occasion, families are allowed to pose questions about their relative’s comfort. One patient, a lifelong hockey fan, was spared from watching endless reels of hockey games when he revealed that he had had enough. But the knottiest emotional and moral questions remain off the table. For instance, Owen says that they won’t ask patients whether they want to live or die until legal experts and ethicists have hashed out the issues. “The problem is, what would you do with the answer?” he says.
… The window onto the patient’s mind closes as soon as the experiment ends. Given the equipment needed and the sophisticated technique of identifying and understanding brain patterns, Owen or his team currently need to be present to do this work. That means that patients can only communicate directly for a limited time. Nonetheless, Owen says the experiments can provide an immense source of relief to the patients’ families. He tells the story of one father who took his son to the movies every week for 17 years. When Owen asked why, the dad said he had a sense his son enjoyed the outings. A Hitchcock screening later confirmed that sense: His son responded to the film with nearly identical spikes of brain activity as a group of healthy patients. “The father did feel that what he’d been doing all these years was worthwhile,” Owen says, “and that was great.”
Illustration by Anna Parini/TED.